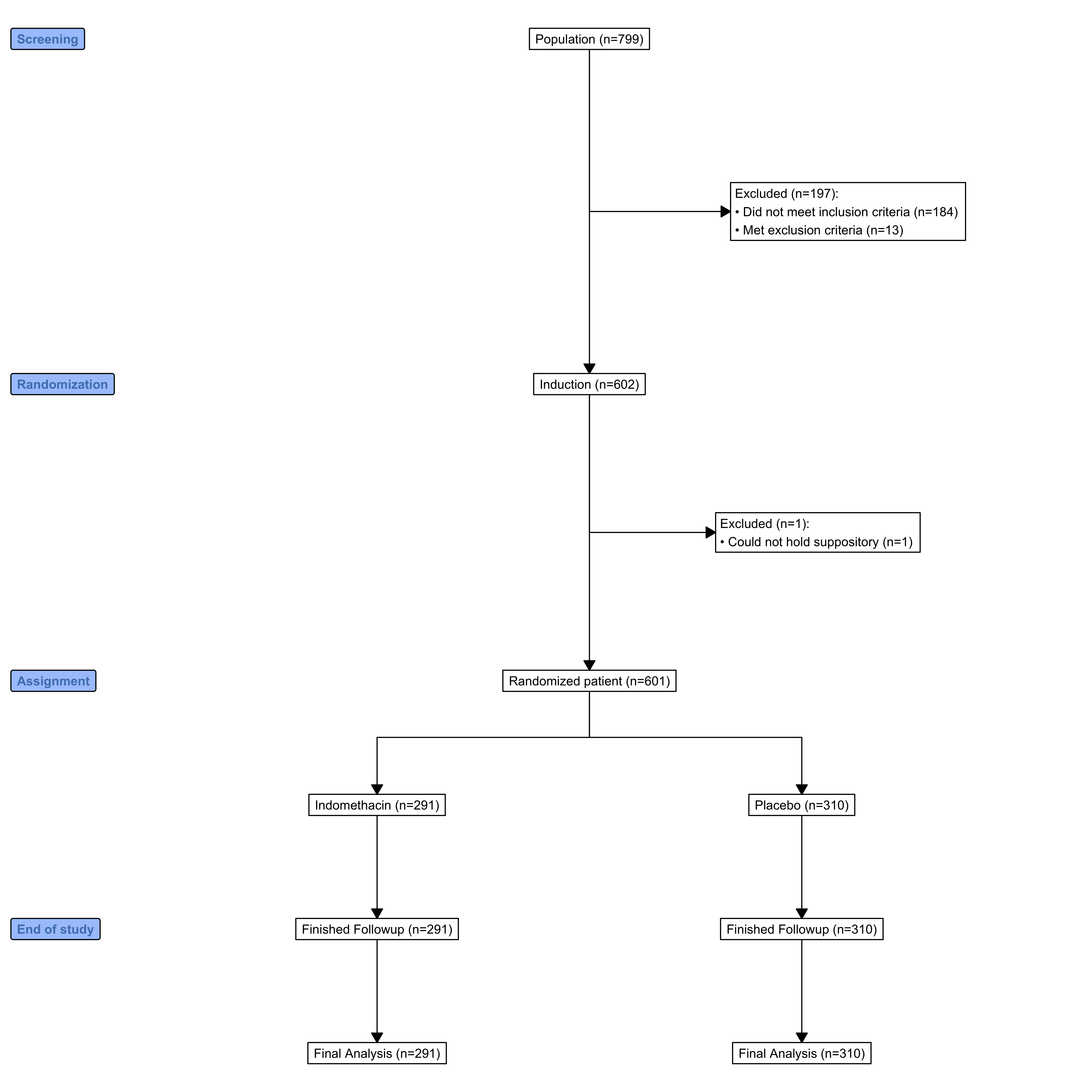
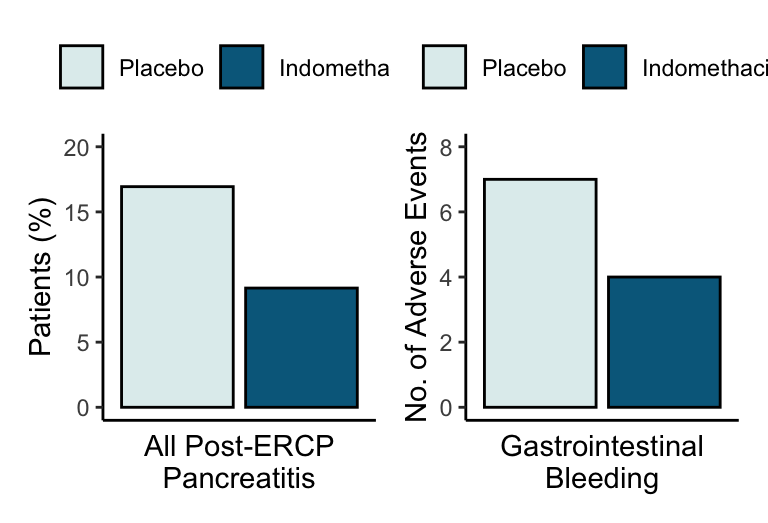
Our findings showed that one dose of rectal indomethacin given immediately after ERCP significantly reduced the incidence of post-ERCP pancreatitis in patients at elevated risk for this complication. Moreover, we found that prophylactic indomethacin decreased the severity of post-ERCP pancreatitis and was associated with a shorter hospital stay. In this trial, the number of high-risk ERCP patients who would need to be treated to prevent one episode of pancreatitis was 13.
The majority of patients in this study had a clinical suspicion of sphincter of Oddi dysfunction, and more than half had sphincter hypertension, as documented on manometry, which suggests that the results are particularly applicable to this challenging patient population. However, among patients who received indomethacin, there was a trend toward benefit with respect to rates of post-ERCP pancreatitis for those who did not have a clinical suspicion of sphincter of Oddi dysfunction (8.5% vs. 20.0%, P=0.11). Moreover, in a subgroup analysis, the relative treatment effect of indomethacin was consistent across the spectrum of patients’ risk of post-ERCP pancreatitis. Additional studies will be necessary to reproduce our results in different patient populations and to determine whether indomethacin is effective in low-risk patients, as suggested by our previous meta-analysis.(Andriulli et al. 2007)
Although more than 80% of the patients in this clinical trial underwent pancreatic stenting on the basis of their elevated risk of post-ERCP pancreatitis, certain patients did not receive stents, either because the endoscopist did not deem it indicated (e.g., difficult cannulation not requiring a precut sphincterotomy) or because placement was not technically feasible (failed pancreatic access). Among patients who received a pancreatic stent, indomethacin reduced the risk of post-ERCP pancreatitis from 16.1% to 9.7% (P=0.04). Indomethacin conferred similar benefit in patients who did not receive a pancreatic stent, reducing the risk of post-ERCP pancreatitis from 20.6% to 6.3% (P=0.049).
Congruent with previous clinical trials evaluating NSAIDs in the prevention of post-ERCP pancreatitis, the risk of adverse events that were potentially attributable to indomethacin in this study was similar in the two study groups. Specifically, there was no significant between-group difference in the frequency or severity of bleeding events. This finding is consistent with previously published data suggesting that NSAIDs in standard doses do not increase the risk of bleeding after biliary sphincterotomy.(Martin L. Freeman et al. 1996; Nelson and Freeman 1994) Of note, patients with contraindications to NSAIDs, such as renal failure and active peptic-ulcer disease, were excluded from this study.
The rate of post-ERCP pancreatitis in the placebo group (16.9%) exceeded that revealed by the internal audit of high-risk ERCP patients at participating institutions (16.9% vs. 10%). (These audit results had been used to calculate the sample size.) This difference may be due to the increased capture of complications that occurs in randomized, controlled trials. Nevertheless, the incidence of post-ERCP pancreatitis in the placebo group of this trial was similar to that in previous studies of NSAID pharmacoprevention in high-risk subjects, in which the mean rate of post-ERCP pancreatitis was 18.8%.(Andriulli et al. 2007)
In summary, prophylactic rectal indomethacin significantly reduced the incidence and severity of post-ERCP pancreatitis in patients at elevated risk for this complication, particularly in those with a clinical suspicion of sphincter of Oddi dysfunction.
Andriulli, Angelo, Gioacchino Leandro, Telemaco Federici, Antonio Ippolito, Rosario Forlano, Angelo Iacobellis, and Vito Annese. 2007.
“Prophylactic Administration of Somatostatin or Gabexate Does Not Prevent Pancreatitis After ERCP: An Updated Meta-Analysis.” Gastrointestinal Endoscopy 65 (4): 624–32.
https://doi.org/10.1016/j.gie.2006.10.030.
Andriulli, Angelo, Gioacchino Leandro, Grazia Niro, Alessandra Mangia, Virginia Festa, Giovanni Gambassi, Maria Rosaria Villani, et al. 2000.
“Pharmacologic Treatment Can Prevent Pancreatic Injury After ERCP: A Meta-Analysis.” Gastrointestinal Endoscopy 51 (1): 1–7.
https://doi.org/10.1016/s0016-5107(00)70377-4.
Cotton, P. B., G. Lehman, J. Vennes, J. E. Geenen, R. C. G. Russell, W. C. Meyers, C. Liguory, and N. Nickl. 1991.
“Endoscopic Sphincterotomy Complications and Their Management: An Attempt at Consensus.” Gastrointestinal Endoscopy 37 (3): 383–93.
https://doi.org/10.1016/s0016-5107(91)70740-2.
Dumonceau, Jean-Marc, Johanne Rigaux, Michel Kahaleh, Carlos Macias Gomez, Alain Vandermeeren, and Jacques Devière. 2010.
“Prophylaxis of Post-ERCP Pancreatitis: A Practice Survey.” Gastrointestinal Endoscopy 71 (6): 934–939.e2.
https://doi.org/10.1016/j.gie.2009.10.055.
Elmunzer, B J, A K Waljee, G H Elta, J R Taylor, S M A Fehmi, and P D R Higgins. 2008.
“A Meta-Analysis of Rectal NSAIDs in the Prevention of Post-ERCP Pancreatitis.” Gut 57 (9): 1262–67.
https://doi.org/10.1136/gut.2007.140756.
Fazel, Ali, Affan Quadri, Marc F. Catalano, Scott M. Meyerson, and Joseph E. Geenen. 2003.
“Does a Pancreatic Duct Stent Prevent Post-ERCP Pancreatitis? A Prospective Randomized Study.” Gastrointestinal Endoscopy 57 (3): 291–94.
https://doi.org/10.1067/mge.2003.124.
Freeman, Martin L. 2007.
“Pancreatic Stents for Prevention of PostEndoscopic Retrograde Cholangiopancreatography Pancreatitis.” Clinical Gastroenterology and Hepatology 5 (11): 1354–65.
https://doi.org/10.1016/j.cgh.2007.09.007.
Freeman, Martin L, and Nalini M Guda. 2004.
“Prevention of Post-ERCP Pancreatitis: A Comprehensive Review.” Gastrointestinal Endoscopy 59 (7): 845–64.
https://doi.org/10.1016/s0016-5107(04)00353-0.
Freeman, Martin L., Douglas B. Nelson, Stuart Sherman, Gregory B. Haber, Mary E. Herman, Paul J. Dorsher, Joseph P. Moore, et al. 1996.
“Complications of Endoscopic Biliary Sphincterotomy.” New England Journal of Medicine 335 (13): 909–19.
https://doi.org/10.1056/nejm199609263351301.
Gross, V, HG Leser, A Heinisch, and J Schölmerich. 1993. “Inflammatory Mediators and Cytokines–New Aspects of the Pathophysiology and Assessment of Severity of Acute Pancreatitis?” Hepato-Gastroenterology 40 (6): 522–30.
HCUPnet, Healthcare Cost. 2019. “Utilization Project. Rockville, MD: Agency for Healthcare Research and Quality, 2016.”
JE, Garcı́a Correa et al. 2007. “Effect of the Administration of Rectal Indomethacin on Amylase Serum Levels After Endoscopic Retrograde Cholangiopancreatography, and Its Impact on the Development of Secondary Pancreatitis Episodes.” Revista Espanola de Enfermedades Digestivas: Organo Oficial de La Sociedad Espanola de Patologia Digestiva 99 (6): 330–36.
Kent, David M, Peter M Rothwell, John PA Ioannidis, Doug G Altman, and Rodney A Hayward. 2010.
“Assessing and Reporting Heterogeneity in Treatment Effects in Clinical Trials: A Proposal.” Trials 11 (1).
https://doi.org/10.1186/1745-6215-11-85.
Khoshbaten, Manouchehr, Homayoun Khorram, Leili Madad, Mohammad Javad Ehsani Ardakani, Haleh Farzin, and Mohammmad Reza Zali. 2008. “Role of Diclofenac in Reducing Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis.” Journal of Gastroenterology and Hepatology 23 (7pt2): e11–16.
Mäkelä, A, T Kuusi, and T Schröder. 1997. “Inhibition of Serum Phospholipase-A2 in Acute Pancreatitis by Pharmacological Agents in Vitro.” Scandinavian Journal of Clinical and Laboratory Investigation 57 (5): 401–7.
Mallery, J.Shawn, Todd H. Baron, Jason A. Dominitz, Jay L. Goldstein, William K. Hirota, Brian C. Jacobson, Jonathan A. Leighton, et al. 2003.
“Complications of ERCP.” Gastrointestinal Endoscopy 57 (6): 633–38.
https://doi.org/10.1053/ge.2003.v57.amge030576633.
Marel, Caroline D. van der, Brian J. Anderson, Janne Rømsing, Evelyne Jacqz-Aigrain, and Dick Tibboel. 2004.
“Diclofenac and Metabolite Pharmacokinetics in Children.” Pediatric Anesthesia 14 (6): 443–51.
https://doi.org/10.1111/j.1460-9592.2004.01232.x.
Murray, Bill, Ross Carter, Clem Imrie, Susan Evans, and Criostoir O’suilleabhain. 2003. “Diclofenac Reduces the Incidence of Acute Pancreatitis After Endoscopic Retrograde Cholangiopancreatography.” Gastroenterology 124 (7): 1786–91.
Nelson, Douglas B, and Martin L Freeman. 1994. “Major Hemorrhage from Endoscopic Sphincterotomy: Risk Factor Analysis.” Journal of Clinical Gastroenterology 19 (4): 283–87.
Singh, Pankaj, Ananya Das, Gerard Isenberg, Richard C. K. Wong, Michael V. Sivak, Deepak Agrawal, and Amitabh Chak. 2004.
“Does Prophylactic Pancreatic Stent Placement Reduce the Risk of Post-ERCP Acute Pancreatitis? A Meta-Analysis of Controlled Trials.” Gastrointestinal Endoscopy 60 (4): 544–50.
https://doi.org/10.1016/s0016-5107(04)02013-9.
Sotoudehmanesh, Rasoul, Morteza Khatibian, Shadi Kolahdoozan, Sanaz Ainechi, Ramin Malboosbaf, and Mehdi Nouraie. 2007. “Indomethacin May Reduce the Incidence and Severity of Acute Pancreatitis After ERCP.” Official Journal of the American College of Gastroenterology| ACG 102 (5): 978–83.
Tarnasky, Paul R., Yuko Y. Palesch, John T. Cunningham, Patrick D. Mauldin, Peter B. Cotton, and Robert H. Hawes. 1998.
“Pancreatic Stenting Prevents Pancreatitis After Biliary Sphincterotomy in Patients with Sphincter of Oddi Dysfunction.” Gastroenterology 115 (6): 1518–24.
https://doi.org/10.1016/s0016-5085(98)70031-9.